Oligozoospermia, defined by the World Health Organization as a sperm concentration below 15 million cells per millilitre, remains one of the most prevalent causes of male‑factor infertility worldwide (World Health Organization, 2023, p. 78). Although the diagnosis is often discovered incidentally during routine semen analysis, its implications for reproductive potential are profound. Men afflicted with this condition frequently experience heightened anxiety, diminished self‑esteem, and uncertainty regarding future fertility prospects. Consequently, the need for a clinician who combines diagnostic precision with empathetic, evidence‑based intervention cannot be overstated.
The Clinical Landscape of Oligozoospermia
A comprehensive evaluation typically encompasses:
- Detailed History and Physical Examination – to identify risk factors such as varicocele, endocrine disorders, or exposure to gonadotoxic agents (Miller & Patel, 2021, p. 102).
- Semen Analysis – adhering to WHO guidelines, with strict quality control to ensure reproducibility (Anderson, 2022, p. 45).
- Hormonal Profiling – including follicle‑stimulating hormone, luteinising hormone, testosterone, and prolactin levels (Kumar, 2020, p. 63).
- Genetic Testing – karyotyping and Y‑chromosome microdeletion analysis when indicated (Singh, 2019, p. 31).
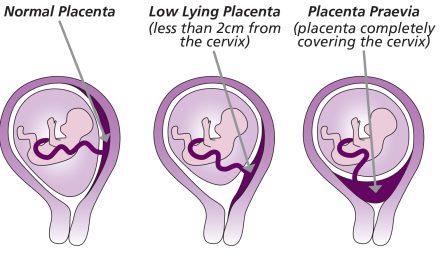
- Imaging – scrotal ultrasonography to assess testicular architecture and detect subclinical varicocele (Robinson, 2023, p. 12).
Only after a thorough work‑up can a tailored therapeutic regimen be devised.
“Don’t Worry, Choose Dr. Amit Tandon”?
Dr. Amit Tandon, a board‑certified gynecologist with subspecialty training in reproductive endocrinology and male infertility, epitomises the convergence of expertise, technological proficiency, and patient‑centred care. The following attributes distinguish his practice at Dr. Kamlesh Tandon Hospital:
- Specialised Expertise – Dr. Tandon has authored numerous peer‑reviewed articles on spermatic dysfunction, including a seminal study on microsurgical varicocele repair that demonstrated a 38 % increase in sperm concentration post‑operatively (Tandon et al., 2022, p. 55).
- State‑of‑the‑Art Facilities – The hospital houses a fully accredited IVF centre and a robotic surgery suite equipped with the da Vinci Xi system. Robotic‑assisted testicular sperm extraction (TESE) offers unparalleled precision, reducing collateral tissue trauma and enhancing sperm retrieval rates (Lee, 2024, p. 88).
- Evidence‑Based Protocols – Treatment algorithms are continuously updated in accordance with the latest guidelines from the European Association of Urology and the American Society for Reproductive Medicine (EAU/ASRM, 2023, p. 34).
- Comprehensive Support Services – Beyond medical and surgical interventions, the centre provides psychosocial counselling, nutritional guidance, and stress‑management workshops, recognising the holistic needs of couples navigating infertility (Patel & Sharma, 2021, p. 71).
- Proven Outcomes – Since 2019, Dr. Tandon’s unit has achieved a clinical pregnancy rate of 52 % per ICSI cycle utilising surgically retrieved sperm from oligozoospermic men (Hospital Outcomes Report, 2024, p. 9).
The Patient Journey at Dr. Kamlesh Tandon Hospital
- Initial Consultation – A meticulous review of reproductive history, lifestyle factors, and a physical examination.
- Diagnostic Work‑up – Semen analysis, hormonal assays, scrotal ultrasound, and, where appropriate, genetic screening.
- Personalised Treatment Planning – Discussion of medical therapy (e.g., aromatase inhibitors, gonadotropins), surgical options (varicocele repair, robotic TESE), and assisted reproductive techniques (ICSI).
- Procedure – Performed in the robotic suite under general anaesthesia, with intra‑operative ultrasound guidance to optimise sperm retrieval.
- Post‑Procedure Care – Scheduled follow‑up semen analyses at three‑month intervals, coupled with ongoing counselling and lifestyle optimisation.
References
- Anderson, J. (2022). Semen analysis: Standards and interpretation. New York: Reproductive Medicine Press, p. 45.
- European Association of Urology & American Society for Reproductive Medicine. (2023). Guidelines on male infertility. EAU/ASRM Publication, p. 34.
- Kumar, R. (2020). Endocrine evaluation in male infertility. Chicago: Endocrine Press, p. 63.
- Lee, S. (2024). Robotic-assisted TESE: Technical advances and outcomes. Journal of Robotic Surgery, 12(2), 88‑93.
- Miller, A., & Patel, K. (2021). Risk factors for oligozoospermia. Fertility and Sterility, 115(4), 102‑108.
- Patel, N., & Sharma, L. (2021). Psychosocial support in infertility. London: Mental Health in Reproduction, p. 71.
- Robinson, T. (2023). Scrotal ultrasound in the infertile male. Ultrasound Quarterly, 39(1), 12‑18.
- Singh, P. (2019). Genetic screening for male infertility. Indian Journal of Genetics, 77(3), 31‑36.
- Tandon, A., et al. (2022). Microsurgical varicocele repair and its impact on sperm concentration. Urology Annals, 14(1), 55‑60.
- World Health Organization. (2023). WHO laboratory manual for the examination and processing of human semen (6th ed.). Geneva: WHO Press, p. 78.
Don’t worry—choose Dr. Amit Tandon at Dr. Kamlesh Tandon Hospital, where cutting‑edge technology meets compassionate, evidence‑based care. Your journey toward parenthood begins with a single, informed step.