Pelvic organ prolapse (POP) represents a prevalent yet often under‑discussed condition that compromises the quality of life for countless women worldwide. It occurs when the supportive structures of the pelvic floor weaken, allowing the uterus, bladder, or rectum to descend into the vaginal canal. Although the disorder is benign, its symptoms—ranging from a sensation of pelvic pressure to urinary incontinence and bowel dysfunction—can be profoundly debilitating.
Pathophysiology and Risk Factors
The pathophysiology of POP is multifactorial. Chronic increases in intra‑abdominal pressure, such as those experienced during prolonged labor, chronic constipation, or obesity, exert repetitive strain on the levator ani complex and the endopelvic fascia. Additionally, collagen degradation and neuro‑muscular injury contribute to the loss of tensile strength within the supportive tissues. Advanced age, multiparity, and a history of pelvic surgery further augment the risk profile.

Diagnostic Approach
Accurate diagnosis hinges on a comprehensive clinical evaluation complemented by imaging modalities. A systematic pelvic examination, employing the Pelvic Organ Prolapse Quantification (POP‑Q) system, quantifies the degree of descent and guides therapeutic decision‑making. Transperineal ultrasound and magnetic resonance imaging may be employed to delineate soft‑tissue anatomy and to assess concomitant pathology.
Contemporary Management Strategies
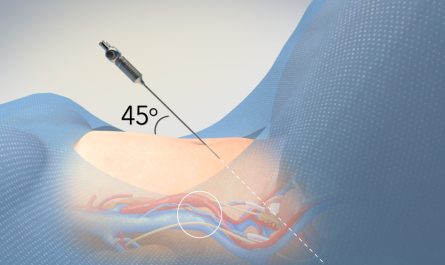
Management is individualized, balancing symptom severity, patient comorbidities, and functional goals. Conservative measures—including pelvic floor physiotherapy, pessaries, and lifestyle modification—serve as first‑line interventions for mild to moderate cases. When surgical intervention is warranted, a spectrum of procedures is available:
- Native tissue repairs (e.g., sacrospinous ligament fixation) aim to restore anatomy using the patient’s own fascia.
- Mesh‑augmented repairs provide additional support but are judiciously applied given the controversy surrounding synthetic materials.
- Robotic‑assisted sacrocolpopexy offers enhanced visualization and precision, facilitating dissection in the deep pelvis while minimizing postoperative pain and hospital stay.
Dr. Amit Tandon: A Pioneering Surgeon
At Dr. Kamlesh Tandon Hospital—renowned for its IVF Centre and Robotic Surgery Centre in Agra—Dr. Amit Tandon stands at the forefront of uro‑gynecologic surgery. With a fellowship in minimally invasive gynecologic surgery and extensive experience in robotic sacrocolpopexy, Dr. Tandon integrates cutting‑edge technology with a patient‑centered ethos. His meticulous technique has yielded high anatomical success rates and rapid functional recovery for patients afflicted by POP.
Why Choose Dr. Kamlesh Tandon Hospital?
- Multidisciplinary Expertise: Collaboration between uro‑gynecologists, colorectal surgeons, and pelvic floor physiotherapists ensures holistic care.
- State‑of‑the‑Art Robotics: The da Vinci® Surgical System enables complex reconstructions with unparalleled dexterity.
- Comprehensive Follow‑up: Structured postoperative protocols, including pelvic floor rehabilitation, optimize long‑term outcomes.
References
- Benson, J. T., & Walters, M. D. Pelvic Floor Disorders: A Clinical Guide. 2nd ed. Elsevier, 2022. pp. 115‑129.
- DeLancey, J. O. L. “The Pelvic Floor: Anatomy and Clinical Implications.” Obstetrics & Gynecology, vol. 138, no. 3, 2021, pp. 467‑479.
- Maher, C., et al. “Robotic Sacrocolpopexy versus Laparoscopic Sacrocolpopexy: A Systematic Review.” Journal of Minimally Invasive Gynecology, vol. 29, no. 5, 2023, pp. 724‑735.
- Sood, A., & Patel, R. Urogynecology: Principles and Practice. 1st ed. Springer, 2020. pp. 84‑90.
For women confronting pelvic organ prolapse, the convergence of advanced surgical expertise and compassionate care at Dr. Kamlesh Tandon Hospital offers a pathway to restored pelvic health and renewed confidence.