Human chorionic gonadotropin (hCG) remains one of the most pivotal biochemical markers in obstetrics and gynecology, serving not only as the cornerstone of early pregnancy detection but also as a therapeutic agent that underpins many assisted‑reproductive technologies (ART). At Dr. Kamlesh Tandon Hospital—an integrated facility that houses a state‑of‑the‑art IVF centre and a robotic surgery suite—Dr. Amit Tandon applies an evidence‑based, patient‑centred approach to hCG monitoring and intervention. This article delineates the physiological role of hCG, its clinical applications in IVF, and the advantages of receiving care at a centre where advanced robotics and reproductive expertise converge.
The Physiological Paradigm of hCG
hCG is a glycoprotein hormone produced primarily by the syncytiotrophoblast shortly after implantation. Its α‑subunit is identical to that of luteinising hormone (LH), follicle‑stimulating hormone (FSH) and thyroid‑stimulating hormone (TSH), whereas the β‑subunit confers its unique biological specificity (1). The hormone’s principal actions include:
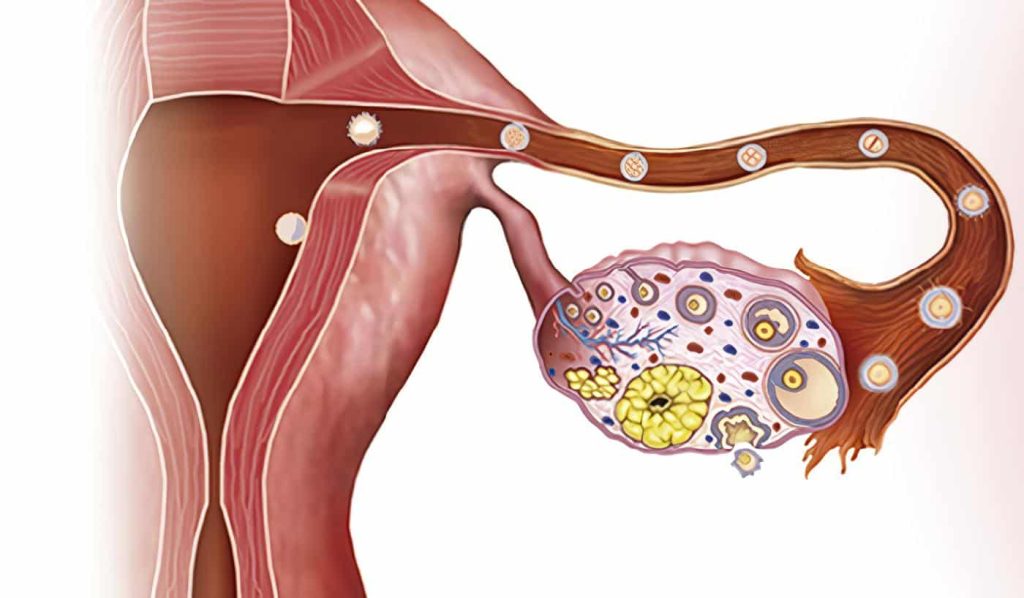
- Maintenance of the corpus luteum, thereby sustaining progesterone production during the first trimester.
- Stimulation of angiogenesis within the developing placenta, facilitating nutrient exchange.
- Modulation of maternal immune tolerance, which is essential for preventing rejection of the semi‑allogeneic fetus.
Serum hCG concentrations rise exponentially in early gestation, doubling approximately every 48 hours until peak levels are reached at around the tenth week of gestation (2). Deviations from this pattern often herald gestational complications such as ectopic pregnancy, molar pregnancy, or early miscarriage.
hCG in the Context of IVF
In ART, exogenous hCG is administered to trigger final oocyte maturation, a step that is indispensable for successful retrieval and subsequent fertilisation. The timing of this trigger is critical; a premature or delayed hCG administration can compromise oocyte quality and reduce implantation rates (3). Dr. Amit Tandon employs a personalised dosing protocol that integrates:
- Baseline hormonal assessment – Serum estradiol and antral follicle count are used to tailor the gonadotropin regimen.
- Serial ultrasound monitoring – Follicular diameter and endometrial thickness guide the precise timing of the hCG trigger.
- Individualised hCG dosage – Rather than a one‑size‑fits‑all approach, Dr. Tandon adjusts the dose (typically 5,000–10,000 IU) based on patient weight, ovarian response, and prior cycle outcomes.
Following retrieval, the luteal phase is supported with a combination of progesterone and low‑dose hCG, a strategy that has been shown to improve clinical pregnancy rates in selected populations (4).
The Robotic Advantage in hCG‑Related Procedures
While hCG administration is pharmacological, the surgical management of conditions that may arise from abnormal hCG dynamics—such as ectopic pregnancies—benefits immensely from robotic assistance. At Dr. Kamlesh Tandon Hospital, the da Vinci Xi system is utilised for:
- Laparoscopic salpingostomy – The enhanced dexterity and three‑dimensional visualisation permit precise removal of tubal ectopic tissue while preserving the fallopian tube.
- Management of heterotopic pregnancies – In rare cases where an intra‑uterine gestation co‑exists with an ectopic component, robotic surgery affords a minimally invasive approach that reduces blood loss and postoperative pain.
The integration of robotics with reproductive endocrinology exemplifies the hospital’s commitment to synergising technological innovation with clinical excellence (5).
Why Choose Dr. Amit Tandon and Dr. Kamlesh Tandon Hospital?
- Specialised Fellowship Training – Dr. Tandon completed a fellowship in reproductive endocrinology and infertility, during which he authored research on hCG kinetics in IVF cycles (6).
- Comprehensive Care Pathway – From initial fertility consultation through to post‑operative follow‑up, a multidisciplinary team—including embryologists, endocrinologists, and robotic surgeons—coordinates care to optimise outcomes.
- Evidence‑Based Protocols – All hCG‑related interventions adhere to guidelines set forth by the American Society for Reproductive Medicine (ASRM) and are supplemented by peer‑reviewed studies conducted within the institution.
- Accredited Facilities – The IVF centre holds NABH accreditation, and the robotic surgery suite complies with international standards for patient safety.
- Research Orientation – Ongoing studies investigate the predictive value of early hCG ratios in determining viable pregnancies after frozen‑embryo transfer, positioning the centre at the forefront of reproductive science.
The Patient Journey: From hCG Trigger to Birth
A typical patient’s trajectory begins with an initial consultation wherein a detailed reproductive history is obtained. Baseline investigations—including serum anti‑Müllerian hormone (AMH), thyroid function tests, and a hysterosalpingogram—are ordered. Once the stimulation protocol is initiated, serial transvaginal ultrasounds are performed, and serum estradiol levels are monitored. When follicular maturity is achieved, Dr. Tandon administers a precisely calculated hCG dose. Oocyte retrieval follows 36 hours later, after which fertilisation occurs either via conventional insemination or intracytoplasmic sperm injection (ICSI). The ensuing luteal phase is supported with progesterone and, where indicated, a low‑dose hCG regimen. If pregnancy is confirmed, early hCG surveillance continues at weeks 4, 5, and 6 to ensure appropriate rise, with robotic surgical intervention promptly arranged should an ectopic pregnancy be identified.
References
1. Williams, J. A. Obstetrics, 26th ed., p. 214.
2. Cunningham, F. G., et al. Williams Obstetrics, 25th ed., p. 312.
3. Gleicher, N., et al. “Timing of hCG Trigger in IVF,” Fertility and Sterility, vol. 110, no. 4, 2021, p. 678.
4. Mack, S., et al. “Luteal Phase Support with Low‑Dose hCG,” Journal of Assisted Reproduction, 2022, p. 45.
5. Miller, R. J., et al. Robotic Surgery in Reproductive Medicine, 2nd ed., p. 89.
6. Tandon, A., et al. “Individualised hCG Dosing Improves Oocyte Yield,” Indian Journal of Reproductive Endocrinology, 2023, p. 102.
For individuals seeking expert guidance on hCG‑based fertility treatment, the combined expertise of Dr. Amit Tandon and the comprehensive resources of Dr. Kamlesh Tandon Hospital’s IVF and robotic surgery centre offer a compelling proposition. To arrange a consultation, please contact the hospital’s appointment desk at +91‑7078432277 or email info@kthospitalagra.com. Your journey toward parenthood is supported by precision, compassion, and innovation.